Book traversal links for A2.2 Information sheet: Practical considerations for implementation of the BD MAX MDR-TB test
Becton Dickinson (BD) has a multiplexed real-time polymerase chain reaction (PCR) nucleic acid amplification tests (NAAT) (BD MAX MDR-TB) for the detection of Mycobacterium tuberculosis complex (MTBC) and resistance to both rifampicin (RIF) and isoniazid (INH) in tuberculosis (TB). For MTBC detection, this test targets the multicopy genomic elements IS6110 and IS1081, as well as a single copy genomic target. For detection of RIF resistance, the test targets the RIF-resistance determining region (RRDR) codons 507-533 of the rpoB gene; for detection of resistance to INH it targets both the inhA promoter region and the 315 codon of the katG gene. The test is performed on the BD Max platform, in which the DNA is automatically extracted and real-time PCR is performed. The World Health Organization (WHO) includes these tests within the class of moderate complexity automated NAATs, and the recommendations below apply to them (1, 2).
WHO recommendations for use
In people with signs and symptoms of pulmonary TB, moderate complexity automated NAATs may be used on respiratory samples for detection of pulmonary TB, RIF resistance and INH resistance, rather than culture and phenotypic drug-susceptibility testing (DST). (Conditional recommendation; moderate certainty of evidence for diagnostic accuracy)
There are several subgroups to be considered for this recommendation:
- The recommendation is based on evidence of diagnostic accuracy in respiratory samples of adults with signs and symptoms of pulmonary TB.
- This recommendation applies to people living with HIV (PHLIV) (studies included a varying proportion of People with HIV). Performance on smear-negative samples was reviewed but was only available for TB detection and not for RIF and INH resistance. Data stratified by HIV status were not available.
- This recommendation applies to adolescents and children based on the generalization of data from adults. Indeterminate results are more likely to be found with paucibacillary TB disease in children.
- Extrapolation for use in people with extrapulmonary TB and testing on non-sputum samples was not considered because data on diagnostic accuracy of technologies in the class for non-sputum samples were limited.
Key performance conclusions
- The BD MAX MDR-TB test performs well for the diagnosis of TB and DR-TB compared with culture and phenotypic DST.
- Limit of detection reported by the company: TB detection = 0.5 colony forming units (CFU)/ mL, RIF/INH detection = 6 CFU/mL.
- The pooled sensitivity and specificity data for the class are presented in the Web Appendix of the WHO consolidated guidelines (3).
Test procedure at-a-glance
- Sample treatment: Raw or concentrated sputum is manually mixed 2:1 with BD MAX STR (sample treatment reagent), shaken and incubated twice, then transferred to a BD MAX MDR-TB sample tube.
- Sample preparation and real-time PCR: The BD MAX MDR-TB sample tube is manually transferred to the BD MAX instrument, which then automates all sample preparation processes (cell lysis, DNA extraction, magnetic bead-based DNA concentration, heat and elution buffer-based DNA purification) and real-time PCR (reagent rehydration and DNA amplification).
- Detection and reporting: Automated by the BD MAX instrument, specific fluorescent probes are used to detect MTBC DNA (IS6110, IS1081 and a single gene target, devR), RIF resistance (RRDR codons 507-533) and INH resistance (inhA promoter and katG codon 315). Results are automatically determined and digitally reported by the instrument within 4 hours.
- Result interpretation: BD MAX automatically reports detection status (detected/ not detected) for MTBC, RIF resistance and INH resistance. RIF and INH may be reported as "unreportable" (i.e. fluorescence not measurable) and INH may have results disaggregated by katG and inhA promoter region targets (mutation detected/ not detected). Also reported are MTBC detection with very low mycobacterial loads without resistance results (MTB low ), lack of sample processing control detection (MTB unresolved), system failure (indeterminate) and incomplete runs (incomplete) (4).
Equipment, supplies and reagents
MDR-TB assay: 24 tests, master mixes, reagent strips, extraction tubes, sample tube, transfer pipettes, septum caps
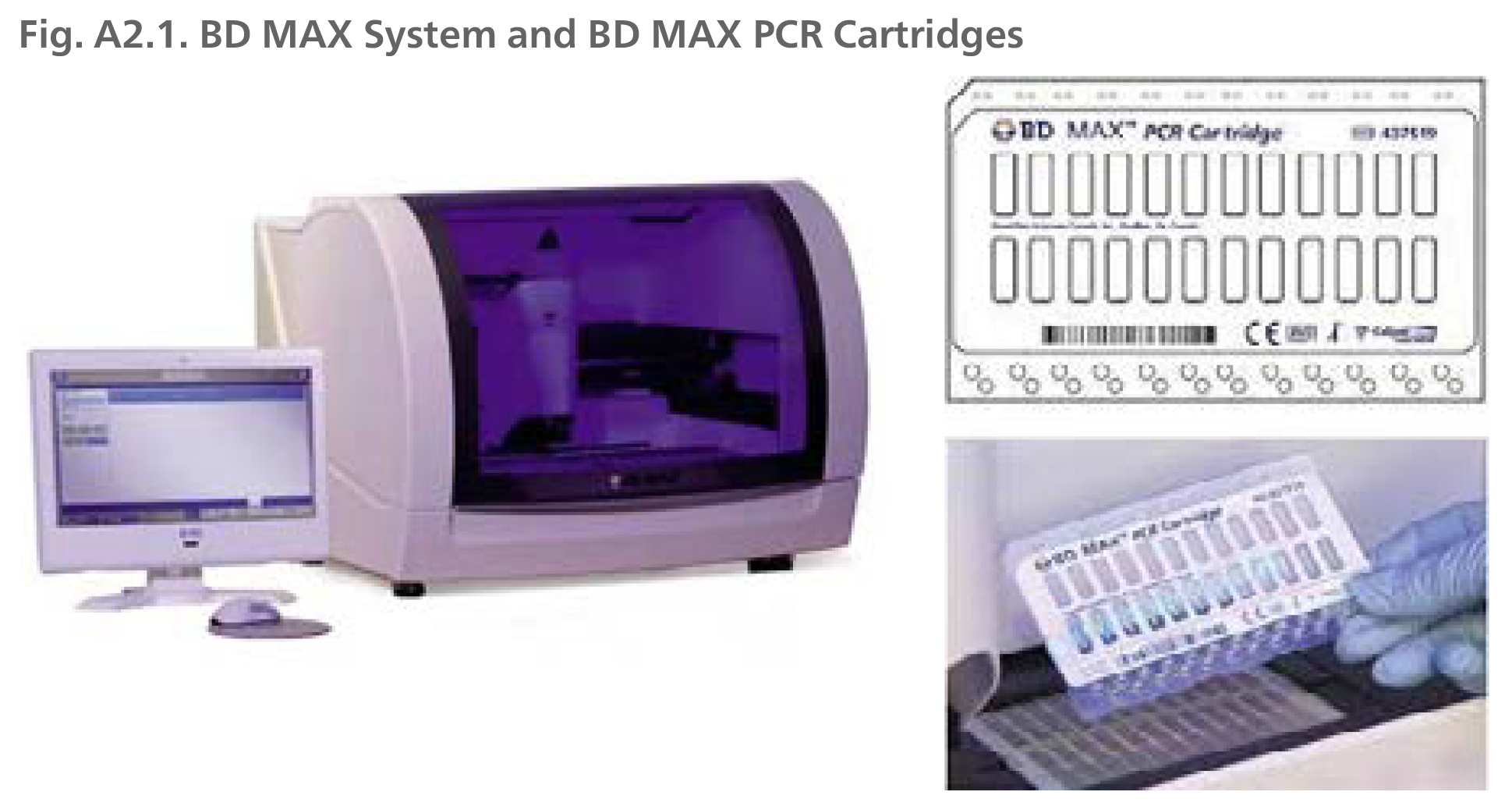
BD MAX system: A fully-integrated, automated instrument that performs nucleic acid extraction and real-time PCR providing results for up to 24 samples per run on a benchtop with a computer
Required, provided separately by BD: BD MAX STR (sample treatment reagent), BD MAX PCR Cartridges (for RT-PCR)
Not provided by BD: Timer (required), personal protective equipment (lab coat, eye protection, powderless gloves), universal power source (UPS; recommmended), waste containers, external controls
Operational considerations
- Testing capacity: 48 tests (24 in <4 hours) per 8-hour workday (4).
- BD MAX system dimensions and weight: The BD MAX system includes a benchtop instrument (94.0 x 75.4 x 72.4 cm, weight of 113.4 kg).
- Sputum storage and testing conditions: For sputum decontamination N-acetyl-L-cysteine/ sodium hydroxide (NALC/NaOH) should be used. Sample processing may be conducted on unprocessed sputum transported at 2-35 °C within 3 days of collection and subsequently stored at 2-8 °C for an additional 7 days. BD MAX STR-treated samples can be stored at 2-8 °C for up to 72 hours and may be retested within this same time period.
- Storage temperature: BD MAX MDR-TB reagents (2-28 °C) and BD MAX instrument (18-28 °C with 20-80% relative humidity).
- Shelf life: At least 9 months.
- Unit prices for low- and middle-income countries: Global prices are not yet available from the Stop TB Partnership Global Drug Facility, but may become available in the future.
Implementation considerations
In addition to the general guidance provided in Section 3.5, consider the following test-specific implementation considerations:
- Area 1 - Policies and planning: BD MAX MDR-TB integration into national algorithms and network placement should consider that (1) the test requires moderate complexity molecular infrastructure, (2) efficient specimen transport may be required to ensure quality sputum specimens are received under appropriate temperature within timelines for BD MAX MDR-TB testing, and (3) any multi-disease testing needs or plans to optimize resource use. Note that the BD MAX system also has assays available to detect Clostridium difficile, enteric bacterial and parasitic pathogens, Group B Streptococcus, methicillin-resistant Staphylococcus aureus (MRSA) and S. aureus, and bacterial vaginosis as well as Chlamydia, gonorrhoea and trichinosis.
- Area 3 - Equipment: The BD MAX system, including the BD MAX instrument and all accompanying reagents, are required for BD MAX MDR-TB testing. Budget planning for test implementation should therefore consider any existing BD MAX systems, available infrastructure and other resource capacities and service and maintenance agreements to ensure optimal system functionality.
- Area 6 - Digital data: Opportunities for diagnostic connectivity solution and e-systems integration may be explored to meet targets established in the Framework of indicators and targets for laboratory strengthening under the End TB Strategy (5).
- Area 7 - Quality assurance: Quality assurance systems and activities for BD MAX MDR-TB mimic those of other moderate complexity automated NAATs. New method verifications should be conducted using a panel of well-characterized M. tuberculosis strains such that sensitivity and resistance for each TB medicine included in the assay (RIF and INH) is represented to demonstrate that the laboratory can achieve expected performance characteristics. Due to potential contamination of the molecular workflow, each run on the instrument must include positive and negative controls to ensure run validity and laboratory spaces should be tested for contamination at least monthly.
- Area 8 - Recording and reporting: Given the potential for decentralized testing sites to report an expanded set of drug sensitivity results for the first time, countries should consider any additional communication routes or reporting procedures that may be required. In addition, diagnostic connectivity solutions may be used to automate reporting.
- Area 9 - Training and competency assessment: As with other molecular drug-susceptibility tests, laboratory staff and clinicians should be trained on appropriate review and interpretation of resistance results for all included medicines.
References for A2.2
- Update on the use of nucleic acid amplification tests to detect TB and drug-resistant TB: rapid communication. Geneva: World Health Organization; 2021 (https://www.who.int/publications/i/ item/update-on-the-use-of-nucleic-acid-amplification-tests-to-detect-tb-and-drug-resistant-tb-rapid-communication).
- WHO consolidated guidelines on tuberculosis Module 4: treatment - drug-resistant tuberculosis treatment. Geneva: World Health Organization; 2020 (https://www.who.int/publications/i/item/9789240007048).
- WHO consolidated guidelines on tuberculosis Module 3: diagnosis - rapid diagnostics for tuberculosis detection. Geneva: World Health Organization; 2021 update (https://apps.who.int/iris/bitstream/handle/10665/342331/9789240029415-eng.pdf).
- BD MAX MDR-TB instructions for use. Franklin Lakes, NJ: Becton Dickinson; 2020 (https://www.bd.com/resource.aspx?IDX=35759).
- Framework of indicators and targets for laboratory strengthening under the End TB Strategy (WHO/ HTM/TB/2016.18). Geneva: World Health Organization; 2016 (https://www.who.int/publications/i/item/9789241511438).
Source: Reproduced with permission of Becton Dickinson, © 2021. All rights reserved.
 Feedback
Feedback